Request Demo
Last update 25 Jun 2025
Nepal Mediciti Hospital
Last update 25 Jun 2025
Overview
Related
6
Clinical Trials associated with Nepal Mediciti HospitalNCT06239233
Gallbladder Infundibulum as a Guide for Ductal Identification in Laparoscopic Cholecystectomy in Nepalese Population at Tertiary Care Hospital
Introduction: Bile duct injury (BDI) is a catastrophic complication of cholecystectomy, and misidentification of the cystic anatomy is considered to be the main cause. Although several techniques have been developed to prevent BDI, such as the "critical view of safety", the infundibular technique, the rates remain higher during laparoscopic cholecystectomy (LC) than during open surgery. Strategy for ductal identification during laparoscopic cholecystectomy can help to prevent laparoscopic bile duct injury.
Methods: A prospective study of 196 patients who will undergo LC during the study period of one year at Nepal Mediciti Hospital will be conducted. The gallbladder infundibulum will be classified by its position located on an imaginary clock with the gallbladder neck as the center point of the dial, 3 o'clock position as cranial, 6 o'clock as dorsal, 9 o'clock as caudal, and 12 o'clock as ventral, as well as the axial position. Patient demographics, pathologic variables and infundibulum classification will be evaluated. Detailed analysis of ductal identification based on gallbladder infundibulum position will be performed in this study. All infundibulum positions will be recorded during intraoperative laparoscopic procedure.
Methods: A prospective study of 196 patients who will undergo LC during the study period of one year at Nepal Mediciti Hospital will be conducted. The gallbladder infundibulum will be classified by its position located on an imaginary clock with the gallbladder neck as the center point of the dial, 3 o'clock position as cranial, 6 o'clock as dorsal, 9 o'clock as caudal, and 12 o'clock as ventral, as well as the axial position. Patient demographics, pathologic variables and infundibulum classification will be evaluated. Detailed analysis of ductal identification based on gallbladder infundibulum position will be performed in this study. All infundibulum positions will be recorded during intraoperative laparoscopic procedure.
Start Date25 Dec 2023 |
Sponsor / Collaborator |
NCT05990569
A Randomized Comparative Study of Pudendal Nerve Block With Bupivacaine Alone and Bupivacaine With Methylene Blue for Postoperative Analgesia in Perianal Surgery
Study Description:
The goal of this clinical trial is to compare the duration of postoperative pain relief achieved with two different approaches to pudendal nerve block in patients undergoing elective perianal surgery. The main question this study aims to answer is whether adding Methylene Blue to Bupivacaine pudendal nerve block can prolong postoperative analgesia compared to using Bupivacaine alone.
Participants in this study will be individuals with ASA I and II physical status undergoing elective perianal surgery under spinal anesthesia. They will be randomly assigned to one of two groups:
1. Group A (Case Group): Participants will receive a pudendal nerve block with Bupivacaine combined with Methylene Blue.
2. Group B (Control Group): Participants will receive a pudendal nerve block with Bupivacaine alone.
The pudendal nerve block will be performed using ultrasound guidance at the level of the ischial spine. The needle tip will be positioned between the Sacro tuberous and sacrospinous ligaments to inject the local anesthetic or the local anesthetic combined with Methylene Blue.
Throughout the study, the researchers will monitor the time to the first rescue analgesic, assess pain levels using the Numeric Rating Scale at various time intervals (2, 6, 24, 48 hours, and 7 days), and observe for any side effects or complications related to the intervention.
Participants will be closely observed after surgery to assess their pain levels and analgesic requirements. The researchers will also evaluate patient satisfaction using the Likert scale.
By comparing the outcomes between the two groups, the study aims to determine if the addition of Methylene Blue to Bupivacaine pudendal nerve block provides superior postoperative analgesia in perianal surgery patients. This information will contribute to the understanding of effective pain management strategies for individuals undergoing perianal surgical procedures and potentially reduce the need for opioids and improve patient outcomes.
The goal of this clinical trial is to compare the duration of postoperative pain relief achieved with two different approaches to pudendal nerve block in patients undergoing elective perianal surgery. The main question this study aims to answer is whether adding Methylene Blue to Bupivacaine pudendal nerve block can prolong postoperative analgesia compared to using Bupivacaine alone.
Participants in this study will be individuals with ASA I and II physical status undergoing elective perianal surgery under spinal anesthesia. They will be randomly assigned to one of two groups:
1. Group A (Case Group): Participants will receive a pudendal nerve block with Bupivacaine combined with Methylene Blue.
2. Group B (Control Group): Participants will receive a pudendal nerve block with Bupivacaine alone.
The pudendal nerve block will be performed using ultrasound guidance at the level of the ischial spine. The needle tip will be positioned between the Sacro tuberous and sacrospinous ligaments to inject the local anesthetic or the local anesthetic combined with Methylene Blue.
Throughout the study, the researchers will monitor the time to the first rescue analgesic, assess pain levels using the Numeric Rating Scale at various time intervals (2, 6, 24, 48 hours, and 7 days), and observe for any side effects or complications related to the intervention.
Participants will be closely observed after surgery to assess their pain levels and analgesic requirements. The researchers will also evaluate patient satisfaction using the Likert scale.
By comparing the outcomes between the two groups, the study aims to determine if the addition of Methylene Blue to Bupivacaine pudendal nerve block provides superior postoperative analgesia in perianal surgery patients. This information will contribute to the understanding of effective pain management strategies for individuals undergoing perianal surgical procedures and potentially reduce the need for opioids and improve patient outcomes.
Start Date12 Aug 2023 |
Sponsor / Collaborator |
NCT05550597
Comparison of the Time to the First Rescue Analgesic Among Parturients Receiving Intrathecal Additive Fentanyl or Intrathecal Fentanyl With TAP Block or TAP Block Alone for Elective Cesarean Sections Under Hyperbaric Bupivacaine Spinal Anesthesia
The postoperative pain management after cesarean section under spinal anestheisa is done using various modalities. The commonly used regimens are systemic NSAIDs/Opioids, USG guided TAP block or Intrathecal additive Fentanyl or combined intrathecal fentanyl and USG guided TAP block.
Investigators aim to compare the postoperative analgesia in terms of time to the first rescue analgesic in parturients receiving intrathecal additive fentanyl only, or intrathecal fentanyl with USG guided TAP block or USG guided TAP block alone for elective CS done under hyperbaric bupivacaine spinal anesthesia.
Investigators aim to compare the postoperative analgesia in terms of time to the first rescue analgesic in parturients receiving intrathecal additive fentanyl only, or intrathecal fentanyl with USG guided TAP block or USG guided TAP block alone for elective CS done under hyperbaric bupivacaine spinal anesthesia.
Start Date15 Aug 2022 |
Sponsor / Collaborator |
100 Clinical Results associated with Nepal Mediciti Hospital
Login to view more data
0 Patents (Medical) associated with Nepal Mediciti Hospital
Login to view more data
99
Literatures (Medical) associated with Nepal Mediciti Hospital01 Jun 2025·Asian journal of neurosurgery
Outcome Determinant of Patients Following Microsurgical Clipping of Ruptured Intracranial Aneurysms
Article
Author: Pokharel, Baburam ; Shah, Damber Bikram ; Paudel, Prakash ; Sharma, Gopal R. ; Joshi, Sumit ; Karki, Prasanna
Abstract:
Objectives Numerous factors can influence patient outcomes following microsurgical clipping of intracranial aneurysms (IAs). Some unique factors, such as aneurysm surgery during the COVID-19 pandemic, also play a role. This study aims to evaluate outcomes in patients with ruptured IAs undergoing microsurgical clipping and identify predictors for both immediate and long-term prognosis.
Materials and Methods This is a retrospective study with prospectively collected data of 500 patients with ruptured aneurysms undergoing microsurgical clipping over a period of 10 years (April 2011–November 2022). The follow-up period ranged from 2 to 10 years, and clinical outcomes were evaluated using the Glasgow Outcome Scale (GOS). Data were analyzed using STATA version 3.10. Logistic regression was used to calculate p-values, with a significance level of p < 0.05.
Results Among 500 patients treated for ruptured IAs, 169 were males and 331 were females, with a median age of 53 years. Postoperative vasospasm was a major predictor of worse outcomes at discharge (p < 0.001), 6 months (p < 0.001), 1 year (p < 0.001), 5 years (p = 0.014), and 10 years (p = 0.006). Patients treated during the COVID-19 pandemic had worse outcomes at 6 months (p < 0.001) and 1 year (p = 0.001).
Conclusion Postoperative vasospasm, intraoperative rupture, and the COVID-19 pandemic were the most important predictors of worse outcomes. Factors such as age, hospital type, Miller Fisher grade, alcohol abuse, diabetes, aneurysm multiplicity, aneurysm size, neck size, ethnicity, hydrocephalus, brain retraction, and lamina terminalis fenestration did not significantly influence the outcomes.
01 Jun 2025·Annals of Medicine and Surgery
Salvage laser lithotripsy for hepatolithiasis in complex biliary anatomy: a case report
Article
Author: Bhat, Pawan Singh ; Rawal, Sushil Bahadur ; Laudari, Uttam ; Acharya, Suyash ; Malla, Srijan ; Rayamajhi, Jyoti
Introduction::
Hepatolithiasis is the presence of gallstones in the bile ducts above the hepatic ducts’ confluence. This condition can cause serious issues like cholangitis and biliary cirrhosis in cases involving post-hepaticojejunostomy. Treatment options for hepatolithiasis include percutaneous transhepatic, endoscopic, and surgical approaches, with laser lithotripsy being effective for difficult stones, and helping to avoid more invasive surgeries like hepatectomy.
Case presentation::
We hereby report a case of a 59-year-old woman with a history of multiple surgeries for hepaticojejunostomy strictures and cholangitis who underwent successful laser lithotripsy for hepatolithiasis.
Discussion::
Hepatolithiasis is particularly prevalent in the Asia-Pacific region. Diagnosis of hepatolithiasis usually begins with an ultrasound, but MRCP provides a more detailed view of the biliary tree, offering better clarity for assessing conditions like biliary dilatation and strictures. Our patient, who had undergone Roux-en-Y hepaticojejunostomy, presented with multiple intrahepatic and common hepatic duct stones along with an anastomotic stricture. Traditional treatments failed to remove the stones. However, IHBR laser lithotripsy via open surgery effectively resolved the issue, demonstrating a successful strategy for complex biliary conditions.
Conclusion::
Laser lithotripsy effectively treats hepatolithiasis in complex biliary anatomy, overcoming challenges when standard treatments fail.
01 May 2025·International Journal of Surgery Case Reports
Laparoscopic Level II thrombectomy for renal cell carcinoma: An index case report from a national tertiary hospital
Article
Author: Adhikari, Mahesh Mani ; Nepal, Umesh ; Khadga, Ajit ; Pokharel, Bharat Mani ; Gharti, Binod Babu
INTRODUCTION:
Renal cell carcinoma (RCC) with inferior vena cava (IVC) thrombosis is a rare and complex condition. Most cases have been managed through open surgery, particularly in premier institutes in Nepal. However, no published literature currently exists regarding laparoscopic management of such cases in this region.
PRESENTATION OF CASE:
We present an index case of right RCC with IVC thrombosis managed laparoscopically at a tertiary cancer center in Nepal. The patient had a history of prior abdominal surgery, which led to dense adhesions complicating the laparoscopic procedure. Despite these challenges, the laparoscopic approach was successfully performed, offering a minimally invasive alternative to traditional open surgery.
DISCUSSION:
The major challenges in this case included managing the dense adhesions from the previous surgery, which significantly hindered the laparoscopic dissection and exposure of the IVC. Additionally, the complexity of tumor removal and IVC thrombectomy posed a significant technical challenge.
CONCLUSION:
Surgical treatment for RCC with IVC thrombus is highly complex, carrying significant risk of peri-operative mortality, and is best performed in a high-volume centre.
100 Deals associated with Nepal Mediciti Hospital
Login to view more data
100 Translational Medicine associated with Nepal Mediciti Hospital
Login to view more data
Corporation Tree
Boost your research with our corporation tree data.
login
or

Pipeline
Pipeline Snapshot as of 24 Dec 2025
No data posted
Login to keep update
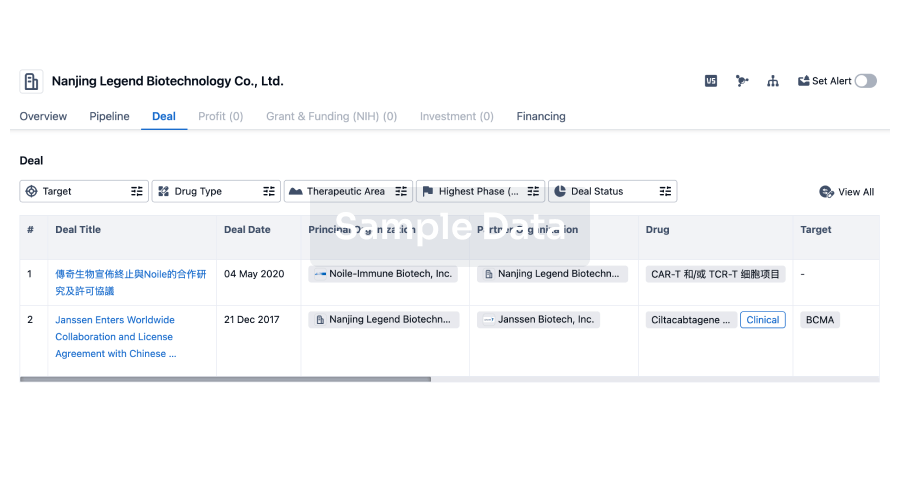
Deal
Boost your decision using our deal data.
login
or
Translational Medicine
Boost your research with our translational medicine data.
login
or

Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or

Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or

Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or

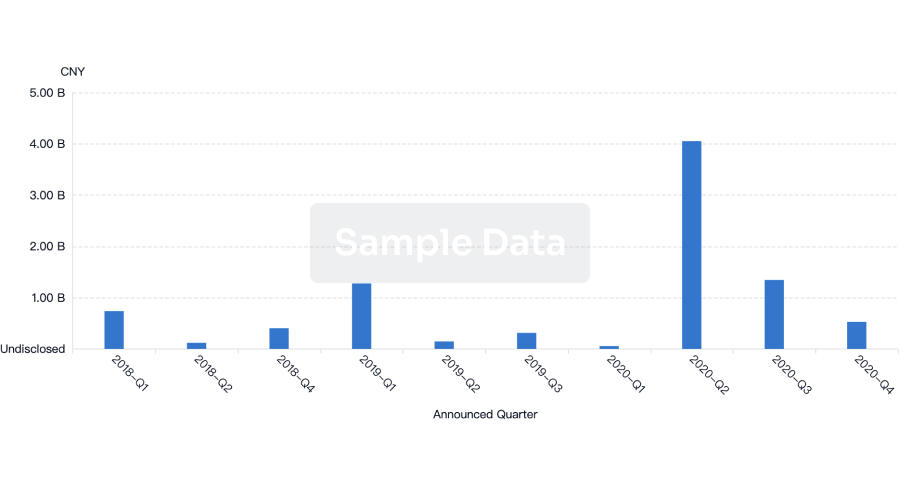
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free