Request Demo
Last update 22 Dec 2025

Khyber Teaching Hospital
Last update 22 Dec 2025
Overview
Related
30
Clinical Trials associated with Khyber Teaching HospitalNCT07111767
Effectiveness of a Modified Cost-Effective Dietary Plan in Promoting Weight Loss and Preservation of Lean Body Mass in Patients After Bariatric Surgery
This study will see if a low-cost dietary plan, based on the standard dietary guidelines of the American Society for Metabolic and Bariatric Surgery (ASMBS) and using locally available foods, can help patients lose weight and keep their lean body mass after bariatric surgery. It will also check if this plan can maintain healthy levels of important nutrients such as vitamin B12, iron, and vitamin D.
Patients who have undergone bariatric surgery will be randomly assigned to follow either the low-cost diet or the regular hospital diet. Their weight, body composition, and nutrient levels will be tracked at baseline, and at 1, 3, and 6 months after surgery.
The aim is to find out if this simpler, affordable diet, which follows international standards, works as well as the regular plan while being easier for low-income patients to follow.
Patients who have undergone bariatric surgery will be randomly assigned to follow either the low-cost diet or the regular hospital diet. Their weight, body composition, and nutrient levels will be tracked at baseline, and at 1, 3, and 6 months after surgery.
The aim is to find out if this simpler, affordable diet, which follows international standards, works as well as the regular plan while being easier for low-income patients to follow.
Start Date01 Oct 2025 |
Sponsor / Collaborator |
NCT07294963
Impact of Lifestyle Interventions on Cognitive Decline in NAFLD: A Randomized Controlled Trial of Liver Fibrosis, Hormonal Imbalance, and Inflammatory Markers
This study investigates whether a structured lifestyle program can help improve thinking skills and liver health in adults with Non-Alcoholic Fatty Liver Disease (NAFLD). We are enrolling 45 participants, aged 18-42, who will be randomly assigned to one of three groups for six months: one receiving general health advice, a second following a supervised Mediterranean diet plan, and a third combining the same diet with a regular walking program. The main goal is to see if these diet and exercise interventions can lead to better scores on memory and reasoning tests, reduce liver stiffness measured by a painless scan (FibroScan), and improve related blood markers of inflammation and hormone balance.
Start Date01 Oct 2025 |
Sponsor / Collaborator |
ACTRN12625001007426
comparison of efficacy and safety of apremilast and methotrexate in moderate to severe psoriasis : a randomized control trial
Start Date15 Sep 2025 |
Sponsor / Collaborator |
100 Clinical Results associated with Khyber Teaching Hospital
Login to view more data
0 Patents (Medical) associated with Khyber Teaching Hospital
Login to view more data
498
Literatures (Medical) associated with Khyber Teaching Hospital01 Dec 2025·Journal of Gastrointestinal Cancer
Comparing ICG-Guided vs. Conventional Laparoscopic Lymphadenectomy in Gastric Cancer: A Systematic Review and Meta-Analysis
Review
Author: Sajjad, Fatima ; Afridi, Abdullah ; Nisa, Farwa ; Khan, Hanifullah ; Shahid, Iqra ; Khan, Muhammad Hamza ; Bacha, Zaryab ; Khan, Iqra ; Khattak, Fazia ; Afridi, Rizwan ; Ali, Muhammad Abdullah ; Kamil, Kamil Ahmad ; Qadri, Maria ; Saleem, Yasir ; Khan, Hafsa ; Habib, Hira
BACKGROUND:
Gastric cancer remains one of the leading causes of cancer-related mortality worldwide, with surgical intervention being a critical aspect of treatment. Lymphadenectomy plays a significant role in managing gastric cancer, with the extent of lymph node removal often influencing survival outcomes. Recent advancements in laparoscopic surgery have introduced the use of indocyanine green (ICG) fluorescence guidance to improve the accuracy and effectiveness of lymphadenectomy. However, the comparative efficacy of ICG-guided laparoscopic lymphadenectomy versus conventional techniques remains a topic of ongoing investigation.
AIM:
This study aims to evaluate the effectiveness and surgical outcomes of ICG-guided laparoscopic lymphadenectomy compared to conventional laparoscopic lymphadenectomy in patients with gastric cancer.
METHODS:
A systematic review and meta-analysis, based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statements, was conducted (PROSPERO: CRD420251039604). A literature review was performed (sources: PubMed, Embase, and Cochrane Library databases; end-of-search date: April 22, 2025) and quality assessment was performed using the ROB 2 and Newcastle-Ottawa Scale. A random-effects model was used to pool the data for the meta-analyses.
RESULTS:
A total of 3996 patients from ten studies were analyzed, with 1870 undergoing ICG-guided surgery and 2126 in the non-ICG group. ICG use was associated with significantly improved 1-year (RR = 1.04) and 2-year (RR = 1.09) overall survival, and a greater number of retrieved lymph nodes (MD = 6.00). While intraoperative blood loss was significantly reduced with ICG (MD = - 14.44 mL), no significant differences were observed in metastatic lymph node count, postoperative complications, operative time, or hospital stay.
CONCLUSIONS:
ICG-guided surgery in gastric cancer is associated with improved short- and mid-term overall survival and enhanced lymph node retrieval. It also significantly reduces intraoperative blood loss without increasing postoperative complications, operative time, or hospital stay. These findings support the clinical value of ICG in improving surgical outcomes.
19 Sep 2025·Cureus Journal of Medical Science
Comparison of Core Decompression and Fibular Strut Graft in Early Avascular Necrosis of the Hip: Assessment of Postoperative Pain and Functional Outcomes
Article
Author: Naqqash, Muhammad ; Afridi, Asif ; Ahmad, Bilal ; Ahmad, Maria ; Yousaf, Haroon ; Khan, Mubbshir ; Ali Jan, Atizaz
INTRODUCTION:
There is limited local data comparing the outcomes of core decompression and fibular strut grafting in early-stage avascular necrosis (AVN) of the hip. International findings may not be directly applicable due to population-specific factors such as genetics, lifestyle, and healthcare access. Early identification of the optimal surgical option is essential for improving patient counseling, postoperative recovery, and overall clinical outcomes.
OBJECTIVE:
To compare postoperative pain and functional outcomes of core decompression versus fibular strut grafting in patients with early-stage AVN of the hip.
METHODOLOGY:
This prospective, randomized comparative cohort study was conducted at the Department of Orthopedic Surgery, Khyber Teaching Hospital, Peshawar, from 14th March 2023 to 13th September 2023. A total of 112 patients aged 18-50 years with Ficat and Arlet stage I-II AVN were enrolled and equally allocated into the core decompression or fibular strut graft groups using blocked randomization. Postoperative pain was assessed at 12 weeks using the visual analog scale (VAS), with a score >3 considered significant. Functional status was evaluated using the Hip Disability and Osteoarthritis Outcome Score (HOOS). Data were analyzed using chi-square tests for categorical variables and appropriate tests for functional scores, with p ≤ 0.05 considered statistically significant.
RESULTS:
Significant postoperative pain (VAS > 3) was observed in 11 (19.6%) patients in the core decompression group and 17 (30.4%) in the fibular strut graft group (χ² = 1.708, p = 0.190). Stratification by age, gender, and BMI consistently showed lower pain rates in the core decompression group, though differences were not statistically significant. HOOS functional scores demonstrated a similar trend favoring core decompression, but these differences also did not reach statistical significance.
CONCLUSION:
Core decompression was associated with fewer patients experiencing significant postoperative pain and showed a trend toward better short-term functional outcomes compared to fibular strut grafting. Its minimally invasive nature may make it a preferable option for early pain management in patients with early-stage AVN of the hip. However, the lack of statistical significance and the short follow-up period warrant further studies with larger sample sizes and inclusion of long-term functional and radiological outcomes before definitive clinical recommendations can be made.
12 Sep 2025·Cureus Journal of Medical Science
The Role of Cortisol and Aldosterone in Hypertensive Nephropathy
Article
Author: Ali, Haidar ; Afnan, Muhammad ; Javed, Qasim ; Mohamed, Ahmed ; Ul Haq, Qazi Taqweem ; Khan, Muhammad Irshad ; Waqas, Taimoor ; Ikram, Wardah ; Mamoon, Muhammad
INTRODUCTION:
Hypertensive nephropathy is a key cause of chronic kidney disease, with both aldosterone and cortisol potentially contributing to its progression. This study investigated the independent and combined effects of baseline and longitudinal changes in serum cortisol and aldosterone levels on the risk and progression of hypertensive nephropathy in patients with essential hypertension.
METHODOLOGY:
A prospective cohort study was conducted at Khyber Teaching Hospital, Peshawar, from January 2022 to December 2023, enrolling 190 adults (30-70 years) with essential hypertension and preserved renal function (estimated glomerular filtration rate (eGFR) ≥60 mL/min/1.73 m², no macroproteinuria). Patients with diabetes, autoimmune disease, chronic infection, adrenal/pituitary disorders, corticosteroid or mineralocorticoid receptor antagonist use, or secondary hypertension were excluded. Fasting blood samples were collected at baseline, 12, and 24 months (8-9 AM) to measure cortisol and aldosterone using chemiluminescent immunoassay (CLIA), with participants avoiding caffeine, smoking, and stress 12 hours prior. Renal function was monitored via serum creatinine, eGFR (CKD-EPI), and urine protein-to-creatinine ratio; hypertensive nephropathy was defined per Kidney Disease: Improving Global Outcomes (KDIGO) as eGFR <60 mL/min/1.73 m² and/or proteinuria >150 mg/day for three or more months. Additional data included blood pressure, BMI, sodium intake, antihypertensive use, smoking, and psychosocial stress. Analyses were performed in SPSS v26.0 (IBM Corp., Armonk, NY, USA) using Kaplan-Meier curves and Cox models (adjusted for confounders). Hormonal interactions were assessed with multiplicative/additive terms, while repeated-measures ANOVA and regression evaluated hormone trajectories.
RESULTS:
Over a median follow-up of 24 months, 43 patients (22.6%) developed hypertensive nephropathy. The absolute risk of nephropathy was substantially higher among those in the highest tertiles of both cortisol and aldosterone (34.4%) compared to those in the lowest tertiles (11.2%). Elevated baseline cortisol levels were independently associated with increased risk of nephropathy (hazard ratio [HR]: 2.31; 95% confidence interval [CI]: 1.29-4.13; p=0.005). Similarly, elevated aldosterone levels were independently associated with risk (HR: 1.97; 95% CI: 1.11-3.50; p=0.021). There was a significant interaction between cortisol and aldosterone levels (p for interaction = 0.038), indicating a synergistic effect on the risk of nephropathy. Patients who developed nephropathy also exhibited increasing hormone levels over time (p < 0.05 by repeated-measures ANOVA). Sensitivity analyses excluding cases occurring within the first six months and stratified by baseline renal status confirmed the robustness of these associations.
CONCLUSION:
Both elevated and increasing serum cortisol and aldosterone levels independently and synergistically predict the development of hypertensive nephropathy. It is suggested that incorporating hormonal profiling into early risk stratification models may enhance identification of hypertensive patients at risk for kidney damage. Future multi-center studies are warranted to validate these findings across diverse populations and to explore whether interventions targeting these hormonal pathways can reduce renal risk.
1
News (Medical) associated with Khyber Teaching Hospital02 Jan 2025
THURSDAY, Jan. 2, 2025 --
Anemia
is prevalent among patients with
rheumatoid arthritis
(RA), according to a study published online Oct. 26 in
Cureus
.
Jamal Shah, M.B.B.S., from Khyber Teaching Hospital in Peshawar, Pakistan, and colleagues examined the prevalence of anemia among 330 patients with RA presenting at a tertiary care hospital in 2023.
The researchers found that more than half of participants had anemia (54.55 percent). The mean hemoglobin level among these patients was 11.41 g/dL, and the red blood cell count averaged 4.26 million/µL. The Disease Activity Score was higher in patients with anemia (mean of 5.23 versus 4.98 in those without anemia). Most people with anemia had elevated C-reactive protein levels (83.33 percent; mean C-reactive protein, 28.79 mg/L) and an elevated erythrocyte sedimentation rate (88.89 percent; mean erythrocyte sedimentation rate, 45.17 mm/hour). There were significant associations observed between anemia and longer disease duration, higher RA severity, and increased inflammatory markers.
"These findings underscore the critical importance of routine screening and management of anemia in RA patients, particularly those with severe or prolonged disease, as addressing anemia could enhance overall patient outcomes and quality of life," the authors write. "Future research should focus on elucidating the mechanisms linking RA and anemia, conducting longitudinal studies to better understand these associations over time, and evaluating the effectiveness of anemia treatments in improving patient health."
Abstract/Full Text
Whatever your topic of interest,
subscribe to our newsletters
to get the best of Drugs.com in your inbox.
Clinical Result
100 Deals associated with Khyber Teaching Hospital
Login to view more data
100 Translational Medicine associated with Khyber Teaching Hospital
Login to view more data
Corporation Tree
Boost your research with our corporation tree data.
login
or

Pipeline
Pipeline Snapshot as of 22 Dec 2025
No data posted
Login to keep update
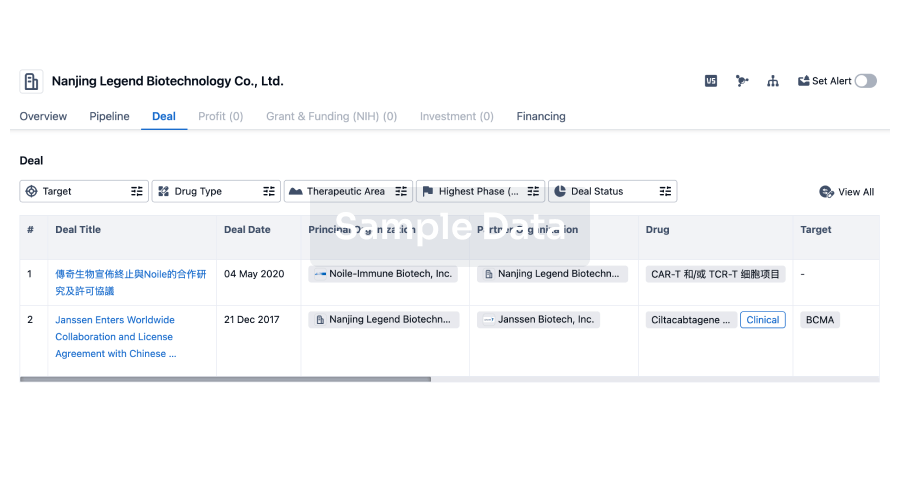
Deal
Boost your decision using our deal data.
login
or
Translational Medicine
Boost your research with our translational medicine data.
login
or

Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or

Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or

Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or

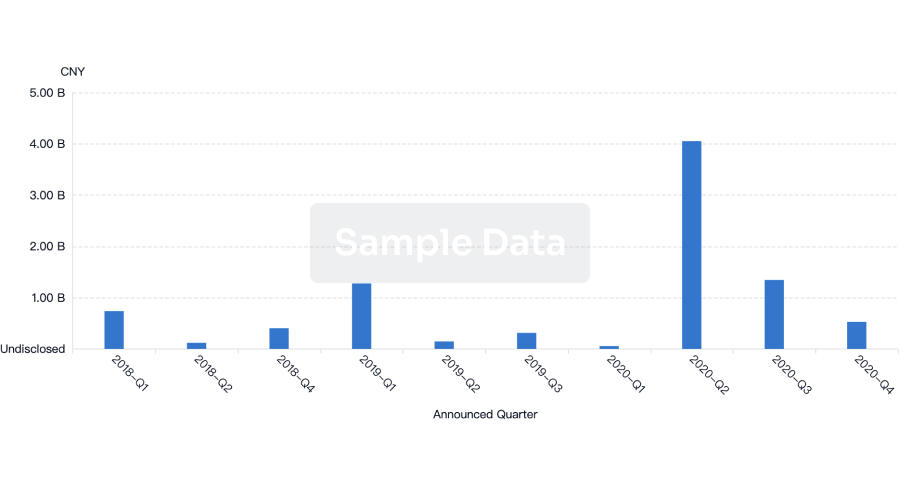
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
